Nothing calls to mind nonsensical treatments and bizarre religious healing rituals as easily as the notion of Dark Age medicine. “The Saturday Night Live” sketch Medieval Barber Theodoric of York says it all with its portrayal of a quack doctor who insists on extracting pints of his patients’ blood in a dirty little shop.
Though the skit relies on dubious stereotypes, it’s true that many cures from the Middle Ages sound utterly ridiculous – consider a list written around 800 C.E. of remedies derived from a decapitated vulture. Mixing its brain with oil and inserting that into the nose was thought to cure head pain, and wrapping its heart in wolf skin served as an amulet against demonic possession.
“Dark Age medicine” is a useful narrative when it comes to ingrained beliefs about medical progress. It is a period that stands as the abyss from which more enlightened thinkers freed themselves. But recent research pushes back against the depiction of the early Middle Ages as ignorant and superstitious, arguing that there is a consistency and rationality to healing practices at that time.
As a historian of the early Middle Ages, roughly 400 to 1000 C.E., I make sense of how the societies that produced vulture medicine envisioned it as one component of a much broader array of legitimate therapies. In order to recognize “progress” in Dark Age medicine, it is essential to see the broader patterns that led a medieval scribe to copy out a set of recipes using vulture organs.
The major innovation of the age was the articulation of a medical philosophy that validated manipulating the physical world because it was a religious duty to rationally guard the body’s health.
Reason and religion
The names of classical medical innovators like Hippocrates and Galen were well known in the early Middle Ages, but few of their texts were in circulation prior to the 13th century. Most intellectual activities in northern Europe were taking place within monasteries, where the majority of surviving medical writings from that time were written, read, discussed and likely put into practice. Scholars have assumed that religious superstition overwhelmed scientific impulse and the church dictated what constituted legitimate healing – namely, prayer, anointing with holy oil, miracles of the saints and penance for sin.
However, “human medicine” – a term affirming human agency in discovering remedies from nature – emerged in the Dark Ages. It appears again and again in a text monks at the monastery of Lorsch, Germany, wrote around the year 800 to defend ancient Greek medical learning. It insists that Hippocratic medicine was mandated by God and that doctors act as divine agents in promoting health. I argue in my recent book, “Embodying the Soul: Medicine and Religion in Carolingian Europe,” that a major innovation of that time was the creative synthesis of Christian orthodoxy with a growing belief in the importance of preventing disease.
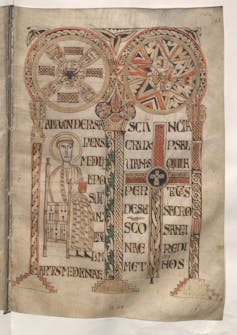
Establishing an intellectual framework for medical study was an accomplishment of early medieval scholars. Doctors faced the risk of being lumped together with those who dealt in sorcery and pagan folklore, a real possibility given that the men who composed the Greek medical canon were pagans themselves. The early medieval scribes responsible for producing the medical books of their age crafted powerful arguments about the respectability and piety of the doctor. Their arguments manifest in illustrations that sanctified the human doctor by setting him parallel to Christ.
This sanctification was a crucial step in including medicine as its own advanced degree program at the first universities that were established around 1200 in Europe. Thus began the licensing of healers: the elite “phisici” – the root of the English word “physician” – trained at the university, along with empirical practitioners like surgeons, herbalists and female healers who claimed a unique authority to treat gynecological illnesses.
Today, religious dogmatism is often equated with vaccine hesitancy and resistance to basic scientific truths like evolution. But deeply religious thinkers of the past often saw rational medicine as an expression of faith, not something endangering it. Herbal remedies were scribbled into the margins of early medieval works on theology, history, church sacraments and more. This suggests that book owners valued such knowledge, and people of all classes were actively exchanging recipes and cures by word of mouth before writing the most useful ones down.
The body in nature
Though the Dark Ages is a period from which no case histories survive, we can still form a picture of an average healing encounter. Texts from that period emphasize the need for the doctor to be highly learned, including being well read in philosophy, logic, arithmetic and astronomy. Such knowledge enabled healers to situate their observations of sick bodies within the rules that governed the constant transformations of nature.
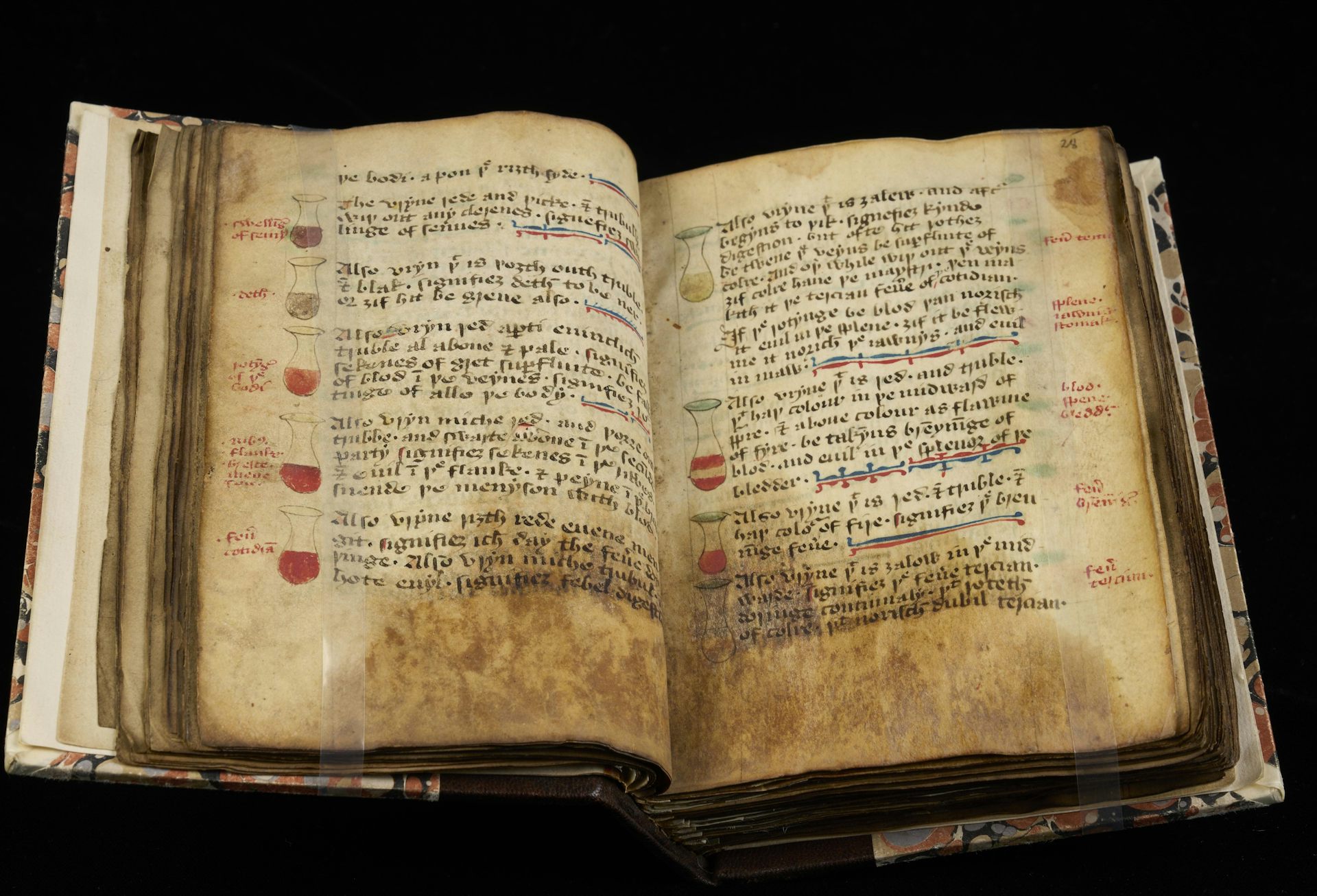
There was no way to perceive the internal state of the body via technology – instead, healers had to be excellent listeners and observers. They sought to match the patient’s description of suffering with signs that manifested externally on the body. The inside of the flesh could not be seen, but the fluids the body excreted – sweat, urine, menstrual blood, mucus, vomit and feces – carried messages about that invisible realm to the outside. The doctor’s diagnosis and prognosis relied on reading these “excreta” in addition to sensing subtle changes in the pulse.
Medieval people were detailed investigators of the natural world and believed the same forces that shaped the landscape and the stars operated inside bodies formed from the same four elements of earth, water, air and fire. Thus, as the moon’s waxing and waning moved the ocean tides, so did it cause humors inside the body to grow and decrease.
The way the seasons withered crops or provoked tree sap to flow might manifest in the body as yellow bile surging in the summer, and cold, wet phlegm dripping in the winter. Just as fruit and meats left untouched began to rot and putrefy, so did dregs and undigested material inside the body turn poisonous if not expelled. Standing water in ponds or lakes generated slime and smell, and so were liquids sitting stagnant in the body’s vessels seen as breeding grounds for corrupt vapors.
In this sense, the menstrual cycle was representative of all bodies, undergoing internal transformations according to seasonal cycles and periodically purged in order to release pent-up fluids.
According to this logic, health depended above all on maintaining the body’s relationship to the physical environment and ensuring that substances were passing through their proper transformations, whether it was food turning into humors, blood disseminating throughout the body, or excess fluids and wastes leaving the body. Bloodletting was a rational therapy because it could help rebalance the fluids and remove toxins. It was visible and tangible to the patient, and, to the extent that we now better understand the placebo effect, it may well have offered some kind of relief.
Fasting, purging, tonics and, above all, monthly dietary regimens were also prominent tools healers used to prevent and relieve sickness. Several medical books, for instance, specified that consuming drinks with cinnamon in November and pennyroyal in August could recalibrate the body’s temperature in winter and summer because one drink was warming while the other was cooling.
Some medieval remedies – such as one produced from wine, cow bile, garlic and onion to heal eye infections – were later proven to be likely effective in treating sickness. But whether these remedies worked isn’t the point. For medieval doctors, vulture brains and cow bile operated according to the same logic that continues to inform research today: Nature operates in mysterious ways, but rational deduction can unlock the hidden mechanisms of disease. The M.D. has direct roots in the Dark Age elevation of “human medicine.”
Before mocking medieval doctors, consider how popular juice cleanses and detox regimens are in the 21st century. Are we really so far from humoral medicine today?![]()
Meg Leja, Associate Professor of History, Binghamton University, State University of New York
This article is republished from The Conversation under a Creative Commons license.
Leave a Reply