
Rural areas across the United States are increasingly offering telehealth services to improve access to quality healthcare for residents who are unable to visit a hospital due to cost or accessibility. In St. Robert, a town of 5,000 in southern Missouri, the telehealth network has been connecting patients to healthcare providers since the 1990s. Improved technology and broadband has made the service more efficient, allowing participants to communicate with live audio and video sessions. Jon Moore, a physician’s assistant at Mercy Clinic Family Medicine in St. Robert, has been practicing dermatology since 1988 when he moved to the town. Moore has noticed an increase in the number of patients who choose to visit their doctors virtually as video technology improved over the years. “We had some big problems when we were first choosing the equipment back in the early 2000s,” Moore said. “A couple of times, telemedicine degenerated into telephone medicine… I ended up describing the lesions over the telephone because we just couldn’t get it going. With the evolution of broadband, it’s gotten better and better.”
Besides the convenience of meeting with a doctor virtually from one’s home, Moore sees many patients who use telehealth because of the cost factor. “If (people) are unemployed, they may not have a car, or if they have a car, they may not be able to afford gas,” Moore told the Columbia Missourian.

“I’ve had patients that were very well insured and were just happy with the convenience of not having to get in a car and drive (to the closest specialist,) and I’ve had others that were just dirt poor or nursing home patients that just couldn’t travel.” There are still uninsured or underinsured patients who can not afford to consult with a specialist like him “so the challenge is there,” Moore said.
Karen Edison, the medical director of the Missouri Telehealth Network, is a dermatologist and frequently hosts teledermatology sessions. “I’m taking care of (patients) through video conference so I see their skin,” Edison said. “They send pictures to me ahead of time and I look at all their skin photos and then I go in the room and talk to them over the computer. It’s just like it is in person, it’s just using technology to bridge distance.” Like Moore, she also notices the improvement in telehealth services due to technology, citing more affordable equipment for both hospitals and patients. “When we first started doing telemedicine, the local rural clinics had to have some very expensive video conferencing equipment,” Edison said. “Today, we use our regular computers. You don’t need to have anything special besides … broadband access to make that secure and high quality.”
“We still have rural areas in Missouri that don’t have high-quality broadband access and this is a problem all over the country in rural areas, but especially in the frontier areas of our country.”
Telehealth requires high-speed and quality broadband, so in many rural areas, a public-private cooperation between government and internet companies is needed. “If you’re talking about live interaction video conferencing, synchronized transmissions, you would need large amounts of broadband both uploading and downloading,” said Rachel Mutrux, the senior program director at the Missouri Telehealth Network.
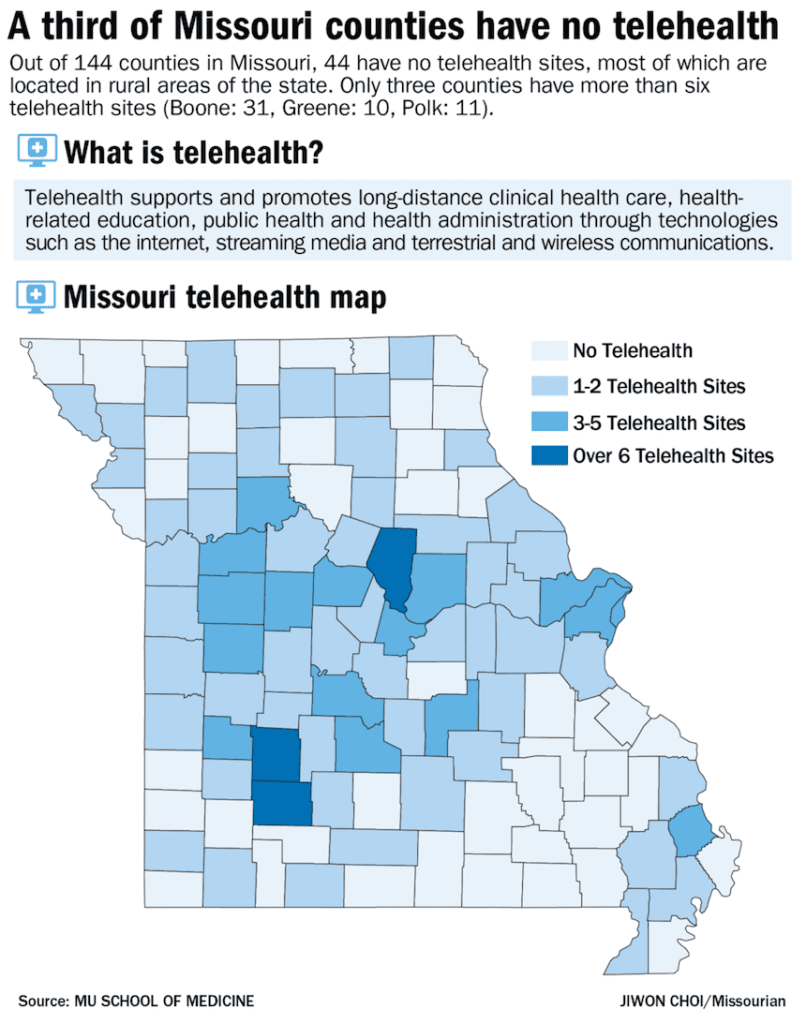
In the early 2000s, some healthcare organizations offering telehealth services as part of the state’s network required a special broadband line installed just for telemedicine. The widespread adoption of electronic health records supported high-speed internet in hospitals being the norm. “Once they started getting electronic health records, they needed a lot more broadband anyway,” she said. “So once they got a lot more broadband anyway, the telemedicine technology got a lot better and didn’t need as much (extra) bandwidth as it did before.” Yet while rural hospitals are improving their broadband access, some telehealth patients still face connectivity challenges, and in those cases, a telephone appointment or an in-person visit is the alternative.
Funding is another challenge for telehealth patients. “When it comes to reimbursement for example, Medicare will only allow reimbursement if the patient is in a specifically designated rural area,” said Mirna Becevic, an assistant research professor of telemedicine at University of Missouri. “This really leaves out urban areas and some other areas that seem rural but do not fall into this category.” “If you think about Medicare patients, they may be in a nursing home and there are so many nursing homes in urban areas that could really benefit from a service like this, so the patient wouldn’t have to leave the nursing home and miss services or meals, but this is not something that Medicare will cover, so it’s a challenge.”
Telehealth supporters in Missouri are also advocating schools to adopt the practice, citing potential reduction in overall healthcare costs in the state. State Representative Kip Kendrick, (D-Columbia) plans to bring up the issue in the 2018 legislative session beginning this month. “Hopefully once we pass additional statues, schools around the state should be able to implement school-based telehealth, where the nurse would facilitate the service in the office connecting with medical specialists on the other end,” Kendrick said. “Children can see specialists for ongoing chronic health conditions in the nurse’s office and may be pulled out of classrooms for 10 to 15 minutes. “Telehealth is already driving down the cost of healthcare and it’s going to become more prevalent in the future,” he said. “Missouri needs to make sure we continue to modernize our statutes, but we need to make sure that people have access to care.”
Leave a Reply