
Office visits for ongoing prescribing of skeletal muscle relaxant drugs tripled from 2005 to 2016, according to a new study from researchers in the Perelman School of Medicine at the University of Pennsylvania.
Moreover, in 2016, nearly 70 percent of patients prescribed muscle relaxants were simultaneously prescribed an opioid — a combination that has the potential to cause dangerous interactions. The researchers also found that muscle relaxants were prescribed disproportionately to older adults during this time period, despite national guidelines warning that this class of drugs should almost always be avoided in patients who are 65 and older. The results were published in JAMA Network Open.
“There are few studies on the short-term efficacy and safety of skeletal muscle relaxants, and almost no data on their long-term effects, so it is very concerning that patients, and particularly older adults, are using these drugs for an extended period of time,” said Charles E. Leonard, PharmD, MSCE, an assistant professor of Epidemiology. “Providers seem to be reaching for them despite incomplete information on their potential benefits and risks.”
Skeletal muscle relaxants are drugs that were approved years ago for short-term treatment of muscle spasms and back pain, and are used today, without good evidence, to treat chronic pain and other conditions. Recommendations generally limit the use of these drugs to a maximum of three weeks, since they have not been shown to work for muscle spasms beyond that duration, and they can cause serious side effects including falls, fractures, vehicle crashes, abuse, dependence, and overdose. Due to these risks, muscle relaxants should be avoided altogether in elderly patients, according to guidelines from the American Geriatrics Society.
Despite these concerns, Leonard and his colleagues hypothesized that the growing opioid epidemic may have led clinicians to prescribe muscle relaxants as an alternative to opioids for long-term pain management.
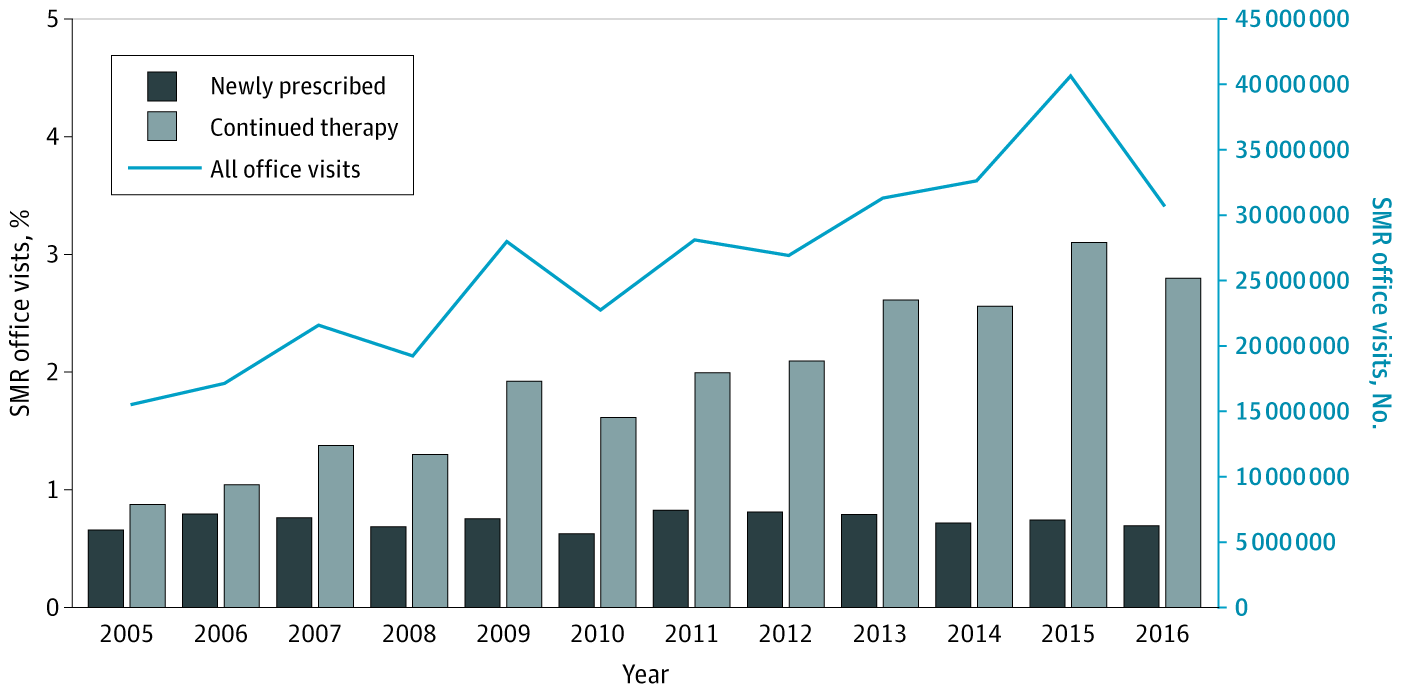
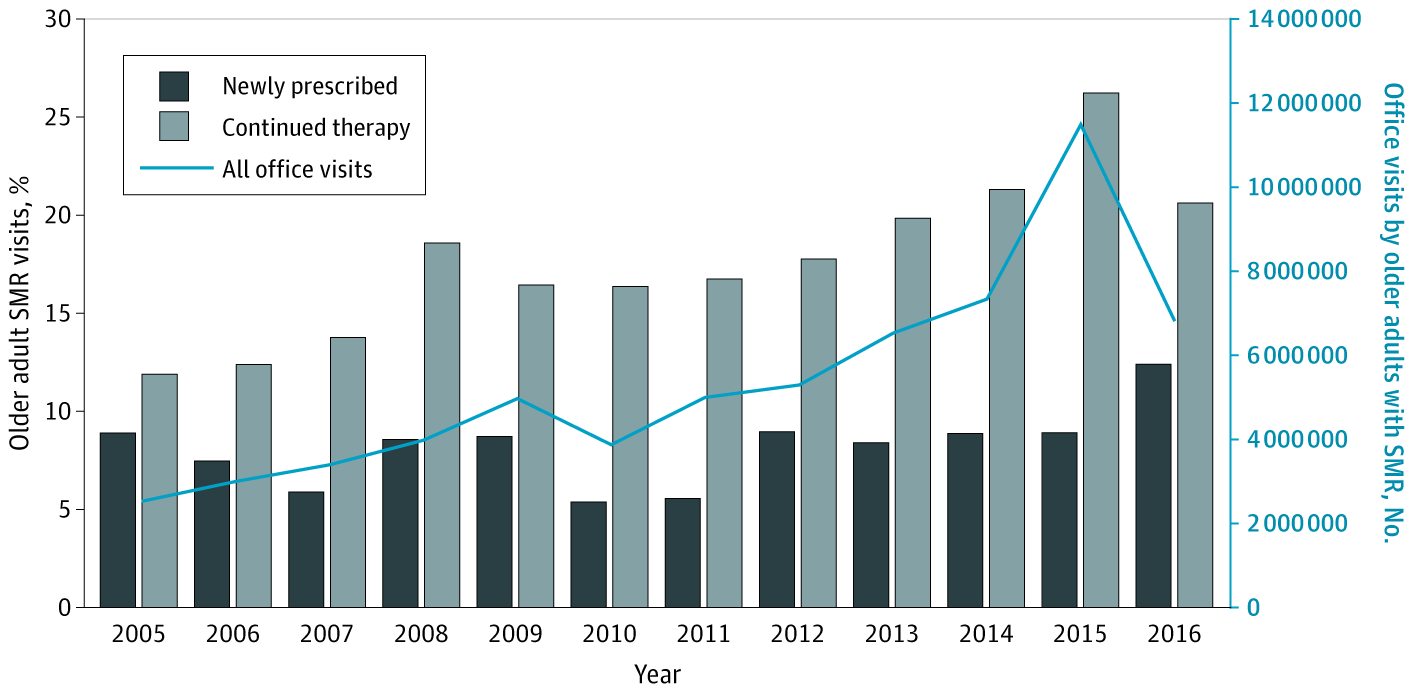
To measure national trends in muscle relaxant prescribing, the researchers analyzed publicly-available 2005-2016 data from the National Ambulatory Medical Care Survey. NAMCS is a U.S.-based annual survey of non-federally funded office-based physicians engaged in direct patient care. The researchers examined the total number of visits per year, and stratified counts by the muscle relaxant agent, whether the drug was newly prescribed or continued therapy, as well as the race, ethnicity, and sex of the patient, and the region of the visit.
From 2005 to 2016, the number of office visits resulting in new muscle relaxant prescriptions remained stable at approximately 6 million per year, while office visits for continued muscle relaxant drug therapy tripled — from 8.5 million in 2005 to 24.7 million in 2016. Worryingly, older adults accounted for 22.2 percent of all muscle relaxant visits in 2016, even though this group accounted for just 14.5 percent of the U.S. population. Also of concern, in 2016, 67 percent of the continued muscle relaxant visits also recorded therapy with an opioid. The U.S. Food and Drug Administration warns against use of co-prescribing of these medications, because of the risk of serious side effects, including slowed or difficult breathing, and death.
“For older adults, I think the message should be to avoid using muscle relaxants, especially when we consider the side effects and increased risk of falls and fractures, and to find alternatives for pain management,” said the study’s first author Samantha Soprano, MPH, a research coordinator and student in Penn’s Master of Behavioral and Decision Sciences program.
Leonard added that, in addition to potential adverse effects, muscle relaxants may not be any more effective in managing pain than medications like Tylenol or Advil. Past studies examining muscle relaxants found they were more efficacious than a placebo, but they were not compared to other therapies. Further research is needed to determine more detailed information about the effects of muscle relaxants, particularly when used for longer periods of time, since their use is so widespread, Leonard said. Additionally, doctors need better, safer options for managing patients’ pain.
“Muscle relaxants’ place in therapy is really limited. Based on most guidelines, they’re normally reserved as second- or third-line therapies,” Leonard said. “Our findings suggest that prescribers may be reaching for these drugs sooner than that.”
Leave a Reply