There’s something for everyone with private health insurance in the American Rescue Plan Act, but determining the best way to benefit may be confusing.
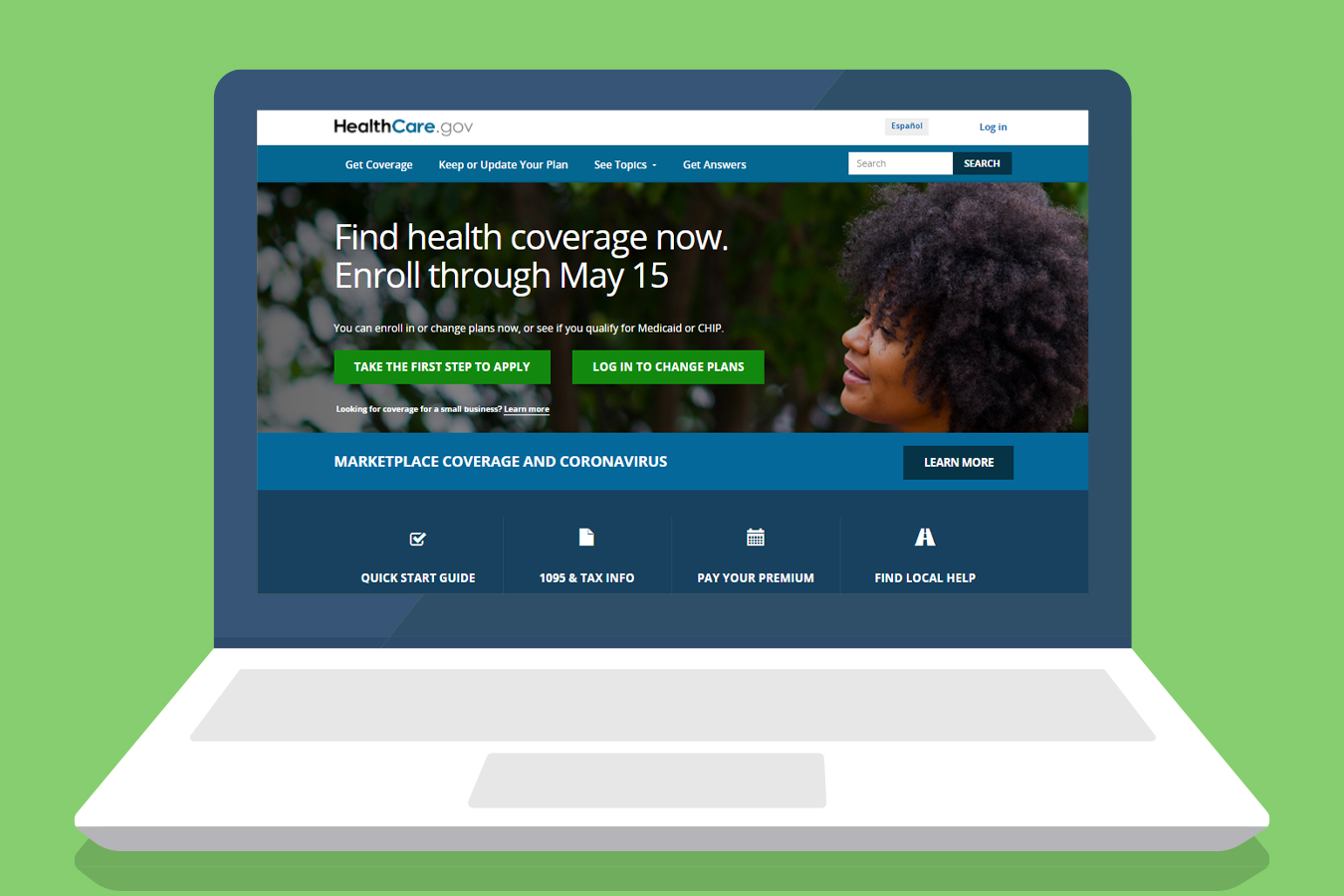
The $1.9 trillion covid relief law that President Joe Biden signed this month will make coverage significantly more affordable for millions of people who either who have marketplace coverage, are uninsured or have lost their employer coverage. In addition, it will eliminate repayment requirements for premium tax credits. Consumers can begin to see those improvements next month, but they may need to go to healthcare.gov and update their application for the changes to take effect then.
Tuesday afternoon, the Biden administration extended the length of time that people have to enroll in or change federal marketplace plans under a covid special enrollment period. The three-month extension means people have until Aug. 15 to sign up and review their options.
The new provisions are temporary; none will extend past 2022 unless Congress acts to make them permanent. Many health care advocates hope that will happen.
“If Congress can circle back and make these improvements permanent, it will go a long way toward making insurance affordable in this country,” said Stan Dorn, director of the National Center for Coverage Innovation at Families USA, a nonpartisan consumer health care advocacy organization.
In the meantime, these provisions will help Americans get or keep their health insurance and provide economic stability as the country emerges from the covid pandemic.
What’s new:
Enhanced Premium Subsidies for Marketplace Plans
When: 2021 and 2022
Who benefits: Just about everyone who has coverage through the Affordable Care Act’s marketplaces. Premium costs for people eligible for subsidies will shrink by $50 per month on average, according to the federal government, but some people will see much larger savings.
Under the ACA, people with incomes between 100% and 400% of the federal poverty level (from $12,760 to $51,040 for one person or $26,200 to $104,800 for a family of four) were eligible for premium tax credits to reduce their premiums for marketplace coverage.
But under the changes passed in the new law, how much people owe is reduced at every income level and capped at 8.5% overall.
For example, a single person who makes $30,000 annually will pay $85 per month in premiums on average under the new law for a silver-level plan instead of $195, according to an analysis by the Center on Budget and Policy Priorities. A family of four making $75,000 will pay $340 rather than $588 per month for similar coverage, the analysis found.
Everyone benefits from the changes, said Tara Straw, a senior policy analyst at the center, including people with incomes above 400% of the poverty level ($51,040 for one person) who were previously not eligible for premium tax credits.
An older customer not yet in Medicare “with an income just over 400% of the federal poverty level in some states would be paying 20% to 30% of their income toward their health care premium,” she said. “Now that will be capped at 8.5%.”
At the other end of the income spectrum, people with incomes up to 150% of the poverty level ($19,140) will owe nothing in premiums. Under the ACA, they had been required to pay up to 4.14% of their income as their share of the premium cost.
Steps to take now:
- People who have marketplace coverage in one of the 36 states that use the federal healthcare.gov platform should go back in and update their applications and reselect their current plan to get new details about their subsidies starting April 1.
- People with marketplace coverage in states that run their own marketplaces should check the procedures there. States including California and Rhode Island, as well as the District of Columbia, have announced they will automatically adjust enrollees’ premiums.
- The enhanced tax credit is in effect for all of 2021 and 2022. For premiums paid for January through April, consumers can claim those premium tax credits when they file their taxes next year.
- People who don’t update their applications now will still be able to claim the additional tax credit amount when their file their taxes in 2022.
- The more generous premium tax credits may mean people can switch to better coverage with lower cost sharing for the same contribution. A potential snag: Switching plans may mean that amounts already paid toward a deductible under the current plan are lost. Check with the insurer.
- People who bought a 2021 plan off the marketplace , perhaps because their income is too high to qualify for premium tax credits, will have to enroll in coverage on the marketplace now in order to get the new premium tax credits, said Straw.
- People who are uninsured can sign up now during the covid special enrollment period that runs through Aug. 15 on the federal exchange. (Individual states have similar special enrollment periods.) People who sign up before April 1 should go back in after April 1 to update their applications.
Free Marketplace Health Insurance for People Who Receive Unemployment Insurance
When: 2021
Who benefits: Anyone who has received or has been determined eligible to receive unemployment insurance benefits in 2021.
Under the American Rescue Plan, anyone who has received unemployment benefits this year will be considered to have income at 133% of the federal poverty level (about $17,000) for the purposes of calculating how much they owe in premium contributions for a marketplace plan. Since people with incomes up to 150% of the poverty level don’t owe anything in premiums under the new law, these unemployed workers can get a zero-premium plan. If they buy a silver-level plan, they can also be eligible for cost-sharing reductions that shrink their deductible and other out-of-pocket costs.
Officials are urging people receiving unemployment insurance to enroll in a marketplace plan now to take advantage of the law’s enhanced premium tax credits. The federal government said the additional savings for people who collect unemployment insurance will be available starting in early July.
Step to take now:
- People who are uninsured or have marketplace coverage can still receive the enhanced premium subsidies described above in the meantime. And because the new law excludes the first $10,200 in unemployment insurance from income for the 2020 tax year, people may be able to qualify for higher premium tax credits based on lower income, Straw said.
No Payback of Excess Marketplace Subsidies
When: 2020
Who benefits: People who earned more money last year than they estimated when they signed up for marketplace coverage.
Under the ACA, people estimate their income for the upcoming year, and the marketplace estimates how much in premium tax credits can be advanced to them every month. At tax time, people reconcile their actual income with their projected income, and if they received too much in tax credits, they generally must pay it back to the government.
The new covid relief bill eliminates that requirement for 2020. The provision could help people who received unforeseen income last year such as hazard pay or perhaps were laid off and hired back as a contractor at higher pay but without benefits, experts said.
Unfortunately, because of the timing of the new law, income tax forms and tax filing software don’t reflect these changes, said Sabrina Corlette, a research professor at Georgetown University’s Center on Health Insurance Reforms.
“A lot of people are going to think they owe money but they’re not going to,” she said.
Steps to take now:
- If you’ve already filed your income taxes for 2020, sit tight. The IRS is reviewing the law and will provide details soon. People should not file an amended tax return at this time.
- If you haven’t yet filed, “some people may want to wait and see if tax software is updated to allow them to file with this adjustment on their tax return,” said Straw. Last week, the IRS announced that the deadline for filing individual federal tax returns for 2020 has been extended this year from April 15 to May 17.
Subsidies to Cover 100% of COBRA Premiums
When: April through September 2021
Who benefits: People who lost their employer-sponsored coverage and want to stay on that plan.
Generally, when people get laid off and lose their employer coverage they can opt to keep it for 18 months, but they have to pay the entire premium plus a 2% administrative fee. This is done under provisions of a law known as COBRA. Under the new law, the federal government will pay the entire COBRA premium through September of this year.
For people undergoing treatment for a medical condition, it can be important to keep their coverage and existing providers. And switching plans midyear can leave people on the hook for a brand-new deductible.
But the newly enacted enhanced premium tax credits and free marketplace coverage for people who collect unemployment insurance make marketplace coverage much more affordable than in the past, experts note.
That could be important because, after September, the new COBRA subsidies will end and people will be responsible for the entire premium, unless the government puts in place a special enrollment period for that circumstance. Without another special enrollment period, they might not be able to get into a marketplace plan until January.
Steps to take now:
- People who missed the original 60-day enrollment window for keeping their job-based coverage can go back and enroll in COBRA now. They have 60 days to enroll after they’re notified of the new provisions under the covid relief plan. They will not owe premiums back to their original eligibility date, but any medical claims they incurred before their enrollment won’t be covered.
- Review coverage to determine whether COBRA or marketplace coverage is the best, most affordable option.
– Michelle Andrews, KHN

Leave a Reply